Premature Baby Care History 1880s-1940s
Footscray World Leader in Premature Baby Care and Reducing Infant Mortality
Introduction to Premature Baby Care History
Premature Baby Care History 1880s-1940s is a family history research project that travelled globally from Footscray in Melbourne’s industrial west to Coney Island’s Luna Park in New York and beyond. The Tweddle Baby Hospital in Footscray was a trailblazer in premature baby care using Sir Truby King’s methods, along with the Plunket and Primrose Nurses. Together they had an extraordinary influence on improving infant mortality. In the United States, Dr Martin Couney, had a remarkable impact on saving hundreds of premature babies from certain death with his bizarre approach.
Preamble
Research for a small talk I gave at my Auntie’s funeral took me on an extraordinary history journey. I became absorbed in the world of premature babies in Australia and overseas circa 1940 and before. My aunt, Margaret KRAKE nee McNISH, was born prematurely on 24 May 1938. She weighed less than five pounds but probably more than three. Babies weighing less than three pounds had little chance of surviving but miracles did happen.
Margaret was born somewhere in “Footscray”. Where I don’t know. Probably not at home. Most likely at a private hospital near the McNISH family home. It could have been ‘Kelvin Grove’, 3 Tongue Street, Yarraville, around the corner from where the family lived. Wherever she was born she needed specialised care as a premature baby until she reached a ‘normal’ birth weight. This could have been at the Tweddle Baby Hospital (‘Tweddle’) on the corner of Gordon and Barkley Streets, Footscray or the place where she was born.
My Father’s Stories
My father, John McNISH told me fascinating stories of Margaret as a newborn and I wanted to explore and confirm these tales. There were many research diversions and I came across information that seemed unbelievable. But it was all true.
The Breast Milk Express
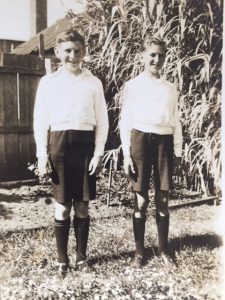
My father told me about the important job he and his brother Bob had in the weeks after his sister’s birth. They were ten and twelve years old at the time and their job was delivering their Mother’s expressed breast milk to the hospital each day. The hospital, whichever one, was a bike ride away. There were no Milk Bar stop-offs or kicking the footy with mates while on this mission.
At a recent 79-year reunion of the Tweddle Baby Hospital in Footscray, one of the patients born in 1939 said that her father rode his bike from Kensington to Footscray with her mother’s precious breast milk. So, the ‘breast milk express’ did happen.
Babes in the Wool
Another story I was able to confirm was that baby Margaret was wrapped from head to toe in cotton-wool. As a child, I imagined my aunt as a baby lying in cotton-wool balls. But of course, that wasn’t the case. Ruth BLUNDELL (nee CAMERON), in her memoir about working at the Tweddle after the second world war wrote:
“These little babies were literally wrapped in cottonwool. Their little legs and arms were bandaged in cotton-wool. A tiny hand knitted woollen singlet was worn over a cotton-wool jacket lined with gauze. A tiny hand knitted bonnet was also lined with gauze and cotton-wool – a frill of cotton-wool edging its tiny face. They really did look beautiful.”[i]
This seemed to be standard practice for premature baby care in other Australian hospitals such as the Royal Women’s in Melbourne at the time. Keeping these babies warm was one of the keys to their survival.
Raised Cots
He also told me that she was kept in a cot that was raised to the ceiling for warmth and only lowered for feeding and changing. I have not been able to confirm this story. Kerrie GOTTLIEBSEN the current Communications Manager at the Tweddle told me:
“There is no record of cots being raised to the roof, and our older staff have never heard of this.”
This makes me think that Margaret was not cared for in the ‘Tweddle’ but in a local private hospital.
Searching for an image of a raised cot led my research further away from Footscray. Each search revealed another extraordinary story of how premature infant care evolved in Australia and overseas from the late 1800s. It was fascinating. There were stories about the Plunket System, Primrose Nurses, incubator babies on display at carnivals, a ‘quack’ doctor who saved the lives of many preterm babies, and an unlicensed nurse who faced a murder charge.
Early Pioneers in Premature Baby Care
Before 1920 babies born prematurely anywhere in the world were given little chance of survival. Most were doomed. They were called weaklings, feeble or “congenitally debilitated” and interest in their special difficulties and care was lost in the dreadful infant mortality statistics of the time. Most premature babies were cared for at home.
First Text on Premature Infant Care – Dr Pierre BUDIN
In 1901 Dr Pierre BUDIN published the first major text on the care of premature infants. Called ‘The Nursling: The Feeding and Hygiene of Premature and Full-term Infants’[ii], it was translated into English in 1907 and became the standard text for doctors and nurses interested in this area of medicine.
However, in these early days, prematurity, was not fully recognised as a medical speciality in paediatrics. A small number of American Hospitals established premature wards, but they didn’t last long and were closed due to lack of interest and funding issues.
Developing Protocols for Premature Infant Care – Dr Julius HESS
In 1922 Dr Julius HESS established a premature infant ward at the Michael Reese Hospital in Chicago where nurses were hired to specifically attend these babies and develop procedures for premature care. It received support from a philanthropic women’s group. Dr HESS also published the first and only book on premature infant care in hospitals, ‘Premature and Congenitally Diseased Infants’.[iii] Incubators were also starting to receive acceptance in the 1920s after early resistance by the medical establishment.
Early Incubator Use – Carnival Entertainment
French doctors were the first to use closed infant incubators to try and reduce the dreadful infant mortality rate and in the late 1880s displays of premature babies in incubators were seen at national fairs and exhibitions.
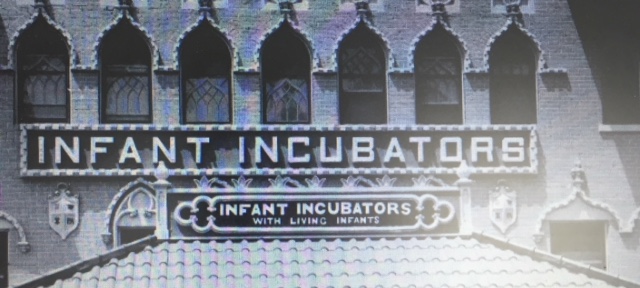
1903 – Coney Island’s Luna Park
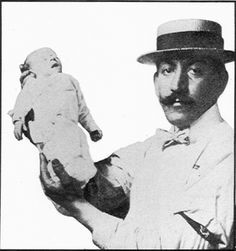
The incubators were taken to America by German immigrant Dr Martin COUNEY but his ideas and the use of incubators were largely dismissed by the medical establishment until the 1920s. COUNEY was forced to do his own thing and he established an infant incubator exhibit at New York City’s Coney Island Luna Park in 1903. The exhibit ran until 1943. He also established one at Dreamland which ran from 1904 until a major fire in 1911.[iv] The Incubator Babies exhibit ran alongside the ‘Freak’ shows of the time including ‘Midget City’ and ‘Lionel the Lion-faced Man’.[v] People were charged to see the ‘show’ and were strangely intrigued and entertained by seeing the tiny babies in poultry like incubators fighting for their lives.
COUNEY was accused of child exploitation and abuse by doctors and groups who wanted to see him closed down. But he persisted with his life-saving work and became as known as the “Incubator Doctor”. He saved many lives over the decades. All babies were accepted by COUNEY, those from parents who couldn’t afford hospital care and those who had been written off by mainstream medicine. He believed all their lives were worth saving. Of around 8,000 babies in his care over the years, he saved 6,500.[vi] The fee-paying public kept the exhibits open by covering all the overhead costs.
1933 Century of Progress Exposition Chicago
The “Living Babies in Incubators” exhibit at the 1933 Century of Progress Exposition in Chicago attracted hundreds and thousands of curious people who paid 25 cents entry fee. This exhibit was a combined effort by Dr Julius HESS and Dr COUNEY who employed six nurses and two wet nurses to care for the babies. COUNEY believed breast milk was best for these under-sized babies and developed a highly nutritious diet for the wet nurses he employed.
1939 New York World’s Fair
By the time the last major incubator exhibit was held at the 1939 New York World’s Fair, incubators had gained approval. The Public Health Department referred premature babies and urged local hospitals to transfer them to the exhibit. Nurses from the Michael Reese hospital staffed the exhibit and parents brought in babies where they were received free of charge.

Kathy Meyer owes her life to Dr COUNEY. She was born eight weeks premature in 1939 and taken to Cornell University’s New York Hospital which had a new training and research centre for premature infants. When it became clear to the Meyers they couldn’t afford the medical bills for their baby to stay in hospital for several months, her paediatrician suggested she go to Martin COUNEY at the New York World’s Fair. COUNEY’s incubator ambulance was sent straight away to collect her. Meyer said:
“I was a sickly baby. If it wasn’t for COUNEY, I wouldn’t be here today. And neither would my four children and five grandchildren. We have so much to thank him for.”[vii]
Dr COUNEY was a trailblazer. He was kind, compassionate and generous and he saved many lives. However, doubts have been raised as recently as 2016 as to whether he actually was a qualified medical practitioner. Read https://www.smithsonianmag.com/history/man-who-pretended-be-doctor-ran-worlds-fair-attraction-saved-lives-thousands-premature-babies-180960200/
Closer to home. We have so much to be thankful for in Australia that our premature babies didn’t have to be commercialised and exhibited in places like Luna Park. We had an infant welfare system from around 1912 and we had the wonderful Tweddle Baby Hospital functioning from 1920 in Victoria.
Infant Mortality from 1900
Infant mortality was a scourge on society. In Victoria, Australia, the situation started to improve after 1920 most likely due to the early developments in establishing an infant welfare system from 1912. The Herald reported on 6 October 1923 that in 1922, 36,288 babies were born. During the first year, 1,936 died (54/1000 births). Over half (or 1,065) died during the first month and of these, 786 babies died in the first week.[viii] Awful statistics, but an improvement on the decade between 1910 and 1920 when the infantile death rate was 69.55 per 1000 births.[ix]
In 1924 New Zealand had by far the lowest infant mortality statistics in the world, 47 per 1000 births. Australia came in second with 63 per 1000. They were far ahead of England and Wales (85/1000); Ireland (86/1000); United States (94/1000); Scotland (98/1000); Belgium (129/1000); and France (132/1000).[x]
These statistics raise questions. Why didn’t the knowledge of the French and Americans, pioneers in writing texts and developing procedures for the care of premature infants, translate into better overall infant survival rates in those countries? And, why did New Zealand lead the world in infant welfare? Many would say the reason for better results in New Zealand was due to Sir Frederick ‘Truby’ KING.
Truby KING and the Plunket Way
Truby KING was a controversial New Zealand medic and health reformer who had strict views on mothercraft and infant welfare. He established the Plunket Society in May 1907 which promoted a ‘scientific approach’ to baby care with rules on feeding, nutrition, hygiene and handling. It was credited with lowering the infant mortality rate in New Zealand from 88 per thousand in 1907 to 32 per thousand in 1937. The Society was named after the first patron, Lady PLUNKET, wife of Lord PLUNKET, Governor-General of New Zealand.
New Zealand had baby hospitals before 1920 which schooled mothers in how to care for their babies. Today the Truby King method would probably be described as ‘Baby Bootcamp’. All aspects of baby’s care were regulated and structured – regular feed times, regular sleeping times, regular bowel movements, no cuddling, no dummies – and it came to Australia, Victoria specifically.
The Society for the Health of Women and Children of Victoria adopted Truby KING’s Plunket system entirely which Miss Lucy MORELAND, explained at the annual meeting in 1920. She told the Society:
“The Truby King system is not a system to deal with disease but one that has as its aim the education of parents …. that they may know and understand the value of simple hygiene and dietetics in relation to child welfare, bearing in mind that this education is necessary for the cultured and well-to-do as it is for the so-called poor and ignorant.”[xi]
She went on:
“In New Zealand we have baby hospitals and hope very soon to open one on similar lines here. These institutions are also schools for Mothers. They can come into residence to learn how to nurse their babies and receive general instruction in mothercraft. If baby is not getting sufficient food, we work up the mother’s supply by simple natural means. Instead of the unhappy, crying infant she brought into hospital the mother takes away with her a happy and contented child, because he is having enough nourishment, has been handled judiciously, fed regularly and trained to sleep through the night.”[xii]
Victoria soon had one – the Tweddle Baby Hospital (‘Tweddle’) – in Footscray. It was established in 1920 as a replica of Truby KING’s famous training hospital in Wellington, New Zealand. General nurses could train there for an Infant Welfare Certificate and graduate as a ‘Plunket’ nurse. Girls without previous experience could do a 12-month course practising on life-sized dolls and graduate as a Baby nurse, or as they were known, a ‘Primrose’ nurse. They were entrusted with the full-time care of one baby becoming a virtual foster mother to their charge. These nurses were named in honour of Maude PRIMROSE, an Australian nurse who went to New Zealand to train in infant care and who became an adherent to Truby KING’s methods.
Miss Ethel May KIRKLAND, a pioneering Plunket Nurse, told the Herald in June 1920:
“I watched infants of premature birth weighing little more than two pounds, develop in a few weeks from miserable specimens of babyhood to healthy normal types. The hospital is more a home than an institution. Any well-planned house with plenty of sunshine, air and open space about it would make an ideal Truby King hospital.
In New Zealand throughout the day all the babies are kept in the open air and many sleep in the open at night. Their cots, ordinary wicker cradles, minus the head cover are placed six feet apart.”[xiii]
Breast Milk or ‘Humanised’ Milk
Truby KING’s number one rule was that babies should be fed the way nature intended with breast milk. Even a tablespoonful a day was preferable to none. If breast milk was unavailable, ‘humanised’ or modified milk was recommended. His milk formula was highly controversial with the paediatric establishment because he reduced the protein in cow’s milk to 1.4% to mimic breast milk. He also claimed all kinds of other milk even buffalo or goat could be brought to the same human milk composition of sugar, fat and protein.
Adherents to the Truby King method believed that it was the best way to reduce infant mortality.
“No social organisation is more worthy of public support than this work of saving babies. The Truby King System is easily the best. Its beneficial influence is amazing and wherever a brand has been established, mothers of all grades of society have eagerly availed themselves of the opportunity to learn how baby should be fed, housed and clothed.”[xiv]
The ‘Independent’, when promoting fund-raising for the local Baby Welfare Centre in Footscray, reported that twelve months after establishing a Truby King Baby Welfare Centre in inner-city Coburg, infant mortality fell from 13.4% to 9.75%.
“Even better results may be anticipated in Footscray and it behoves everybody who loves a baby to give liberally.” [xv]
They were right, in 1938, the year my Aunt was born, Footscray had the lowest infant mortality in the world![xvi]
The Footscray Plunket rooms were in Nicholson Street.[xvii] Quite apart from educating mothers on the best nutrition for their baby, educating them about simple hygiene alone helped reduce the incidence of infantile diarrhoea, one of the biggest killers of children under one year.
The Truby KING Way Today
Truby KING’s system was successful in its time but it’s doubtful if his disciplined and controlled approach to baby care and parenting would be acceptable today. His emphasis on breastfeeding and nutrition is certainly still relevant. However, his conservative belief system in relation to the role of men and women in society which underpinned his ‘scientific’ approach to motherhood would probably get the thumbs down.[xviii] He still has a place in history, and he is certainly remembered in New Zealand as a great public figure. Today Tweddle has an expanded role in Victoria’s family and community health care services but its genesis lies in the methods and crusade of one man, Sir Truby KING and his disciples.
Tweddle Baby Hospital – The Beginning
A small group of people – a nurse, a doctor and a politician – concerned about the appalling infant mortality statistics in the first two decades of the 1900s decided to do something about it. Plunket Sisters controlled infant welfare centres in Coburg and Footscray but there was nowhere to train additional nursing sisters in the Truby King methods.
Nurse, Miss Maude PRIMROSE a devotee of Truby King, Dr J. W SPRINGTHORPE a lung and heart specialist and the Hon. J. HUME, approached businessman and philanthropist, Mr Joseph TWEDDLE for help. Mr TWEDDLE had property to spare but it was in Greensborough, too far away on the outskirts of Melbourne.
Mr GENT, the Town Clerk of Footscray and Mr J LEVY were brought into negotiations which led to Footscray Council granting a site on the busy corner of Barkley and Gordon Streets. Mr TWEDDLE donated £3,000 to get building construction started and guaranteed an overdraft to £7,000.
Location Didn’t Matter – Education Saved Lives NOT the Environment
The baby hospital was on the main bus and transport route into Footscray and the city of Melbourne. It was also across the road from the Footscray Football Club Oval. Not only was the hospital on one of the busier intersections in Footscray, but Footscray was also the heart of industrialised Melbourne. Nearby industries included: bone dust and manure-works; abattoirs and meat preserving; glue, tallow and oil makers.[xix] All sending their pollution into the air and down the Maribyrnong River. But the location didn’t concern the Tweddle campaigners. They claimed:
“Infant health was threatened more by ignorant mothers rather than the environment itself.”[xx]
Miss Lucy MORELAND, who addressed the Society for the Health of Women and Children of Victoria, in 1920 was brought over from New Zealand to be Matron. She was so dedicated to the success of Tweddle that she worked for the first six months without pay.
Snapshots of Premature Baby Care in Hospitals and Homes before 1940
The Tweddle Baby Hospital
At Tweddle, the premature babies had their own separate nursery. Ruth BLUNDELL (nee CAMERON) remembers:
“Little cots were small wicker baskets on a cane frame – painted white. They could be wheeled out. They were made up the same way as the larger cots with a hot water bottle placed between the mattress and the chaff mattress. Another hot water bottle was sometimes placed behind the baby and tucked in the ‘enveloper’ (a blanket that came up from under the mattress and then over). Later the hospital was able to purchase an electronically heated, thermostatically controlled metal cot.”
“They learned to suck from a tiny bottle with a soft rubber mouthpiece. If they did not manage to suck at first, they were tube fed. Feeding was usually 3-hourly during the day and night, preferably with breast milk expressed by the mother. If this was not possible a specially modified formula was used.”[xxi]
Carried under a mid-wife’s coat
In 1932 there was a report in The Herald that Stanley James MOORE, a 2lbs 14oz baby at birth was now doing well at the Tweddle. The report said:
“Born on April 30, one of the coldest mornings of the year. He was taken to the Tweddle Baby Hospital from the Queen Vic, wrapped in cotton-wool and carried under the midwife’s coat, half an hour after he was born.
A premature basket cot lined with brown paper and heated with hot water bags kept his temperature up until he was large enough to leave it.”[xxii]
Sister Purcell – The Art of Caring and Managing a Premature Baby
If you didn’t have access to a hospital and gave birth prematurely in a rural area your baby would be lucky to survive. Sister Purcell, author of ‘The Australian Baby’[xxiii] wrote a series for the rural newspaper, the ‘Weekly Times’ in 1932 about caring for a premature baby. She said:
“The care and management of the premature baby is an art in itself.”[xxiv]
Survival depended on four areas requiring meticulous preparation and attention before and after baby’s birth. I’ve summarised Sister Purcell’s advice below.
Keep Them Warm – A Home-made Incubator
Baby must be kept warm because he cannot maintain his own body temperature. A constant 70°F must be maintained in an airy room.
Have at the ready a cot lined with brown paper or a home incubator made with two clothes baskets one larger than the other, or a cardboard box with holes placed in an ordinary basinet. The outer basket lined with a soft wool blanket and an inner basket similarly lined placed inside. A soft chaff mattress is placed in the inner basket with a covered hot water bottle. Hot water bottles should then be placed between the blankets at the foot and one on either side of the bed; the foot bottle should be about 20°F hotter than the two side bottles.
The bottles should be refilled in rotation to keep the temperature even. A dairy thermometer should be used to ensure the cot temperature is kept at about 95°F or whatever is necessary to keep baby’s body temperature at 99°F.
Have soft absorbent wool ready to wrap the baby including a little jacket and bonnet made of wool covered with muslin and soft bandages to bind the wool around the arms and legs
Avoid Unnecessary Handling
Immediately after birth wrap baby in a piece of absorbent wool and place him in the prepared bed. Leave baby undisturbed for several hours to allow recovery from the effort of being born and handle baby as little as possible after that. Baby is oiled all over with warm olive oil every 2-3 days without being removed from the bed to avoid chilling. There is no bathing until baby can maintain his own body temperature.
Avoid Infection
To minimise the risk of infection no-one should be in baby’s room except the mother and person in attendance. Children especially should be kept away and people who are not well. A small infection would be lethal.
Careful Feeding
For the first 24 hours, nothing is necessary except boiled water given by dropper. Expressed breast milk is best as it’s easily digested and highly nutritious. It should be obtained at any cost and can be fed by a medicine dropper. If unavailable from Mother, then from a healthy nursing mother.
Another piece of artful nursing advice from Sister Purcell.
“If baby is strong enough to suck the double cot must be carried to the Mother’s bed and she must lean over it and not lift baby from the cot while nursing.”[xxv]
The Dionne Quintuplets – Canada
The Dionne Quintuplets caused a worldwide sensation when they were born near the village of Corbeil in Ontario on 10 May 1934. They were 8 weeks early and their total weight was 13lbs 6 ozs. Mother Elzire thought she was having twins and went into shock after the identical baby girls were born. The babies were kept in a wicker basket covered with heated blankets and placed by the open door of the stove to keep them warm.
“One by one, they were taken out of the basket and massaged with olive oil. Every two hours for the first twenty-four, they were fed water sweetened with corn syrup. By the second day they were moved to a slightly larger laundry basket and kept warm with hot-water bottle. They were watched constantly and often had to be roused. They were fed the ‘seven-twenty’ formula: cow’s milk, boiled water, two spoonfuls of corn syrup, and one or two drops of rum for a stimulant.”[xxvi]
I doubt this formula would have won approval from the Plunket nurses at the Tweddle in Footscray.
The babies were transferred to a hospital because the Weekly Times reported on 4 August 1934 that they were still in incubators at two months. There was a proposal to exhibit them at the Century of Progress Exposition in Chicago, but it was vetoed by their doctor Dr DaFoe. Instead, picture postcards were sold.[xxvii]
Queenie’s Private Hospital Altona
In the 1920s expectant mothers living in Altona relied on the service of an unofficial nurse and hospital in Queen Street, Altona. The ‘Waverly Private Hospital’ was owned and operated by Sylvia Evelyn KOCH (or COOK) otherwise known as ‘Queenie’. A Williamstown doctor visited the hospital twice a week to check on patients.
Queenie was unqualified and was arrested on multiple charges with being an unlicensed nurse. She’d had several run-ins with the law and had even faced a charge of causing the death of a patient. After a court case in 1930 and being fined in 1931, she picked up sticks and opened a nursing home in Seddon. She eventually moved to Footscray where she continued to deliver babies until she opened a pub in Seymour.
Queenie’s daughter remembers:
“She wore a veil although no formal training and she assisted in delivery of babies and with operations.
I lived there at the ‘hospital’ with my brother Frank and Mother and Father. Dad (Joe) had built the house/hospital and assisted with the cooking. He also looked after the little premature babies after he was laid off from work. Mum (who was also known as ‘Queenie’) would put the premature babies into a shoe box and rested the box on the oven which had to be kept just warm – not too hot and not too cold. This was Dad’s responsibility. He would sit and watch over the babies and adjusted the temperature, Mum fed the premature babies a mixture of two drops of brandy mixed with boiled water which she fed them with an eye dropper. She saved many babies like that – she lost some and that was always a sad occasion.”[xxviii]
Maybe ‘Queenie’ delivered my Auntie Margaret in Footscray on 24 May 1938.
Margaret was a beautiful person in every way. She was always so kind, generous and compassionate towards her family and friends. Despite her delicate start, she thrived and went on to live for eighty wonderful years.


[i] Blundell, Ruth (nee Cameron) (2007), The Tweddle Baby Hospital and School of Mothercraft. A Memoir.
[ii] http://www.neonatology.org/classics/nursling/nursling.html
[iii] https://babel.hathitrust.org/cgi/pt?id=uc2.ark:/13960/t8pc39x0z;view=1up;seq=7
[iv] Ibid
[v] https://www.thevintagenews.com/2018/06/06/coney-islands-craziest-ever-exhibit/
[vi] https://bklyner.com/remember-when-incubator-babies-were-a-coney-island-attraction-bensonhurst/
[vii] https://www.smithsonianmag.com/history/man-who-pretended-be-doctor-ran-worlds-fair-attraction-saved-lives-thousands-premature-babies-180960200/
[viii] The Herald, Saturday 6 October 1923, p23
[ix] The Herald, Thursday 2 April 1936, p14
[x] Numurka Leader, Wednesday 7 August 1929, p6
[xi] The Herald, Tuesday 14 December 1920, p9
[xii] Ibid
[xiii] The Herald, Tuesday 22 June 1920, p4
[xiv] Independent (Footscray), Saturday 13 August, p6
[xv] Ibid
[xvi] The Herald, Monday 14 February 1938, p6
[xvii] Ibid
[xviii] http://www.nzjh.auckland.ac.nz/docs/1981/NZJH_15_1_02.pdf
[xix] Codognotto, Kathleen & Crow Collection Association (1992), History of Children’s Services in the Western Region – Regulating Footscray Mothers: The Tweddle Baby Hospital and the Plunket System.
[xx] Ibid
[xxi] Blundell, Ruth (nee Cameron) (2007), The Tweddle Baby Hospital and School of Mothercraft. A Memoir.
[xxii] The Herald, Wednesday 27 July 1932, p4
[xxiii] This book is “missing” from the National Library of Australia Collection
[xxiv] Weekly Times, Saturday 16 April 1932, p21; Saturday 23 April 1932, p22; Saturday 30 April 1932, p24; and, Saturday 7 May 1932, p21
[xxv] Weekly Times, Saturday 30 April 1933, p24
[xxvi] https://en.wikipedia.org/wiki/Dionne_quintuplets
[xxvii] Weekly Times, Saturday 4 August 1934, p9
[xxviii] Caesar, Ann et al, ‘A Bush Hospital by The Bay: Altona Hospital 1932 to 1996, Altona – Laverton Historical Society Inc. 2018
Hi, interesting site. Can anyone tell me how they resuscitate a baby whos heart had stop during birth in 1940? My brother was born a blue baby because his cord was around his neck, he lived.
Very interesting history, thank you for posting. My father was born 2 months early in 1948, and my son was born last year nearly 3 months early. Medical science has come SO far!
Thank you Marie. It was so interesting researching the story. I could barely believe what I was reading at times. We really do have to be so grateful for the advances in medical science.